The healthcare field has become increasingly complicated due to various professional groups, each with its own characteristics, methods, and new procedures. Interoperability in healthcare is necessary to ensure the system’s long-term stability. For this reason, some health information technologies have been developed over the last few decades to convert paper-based health information into electronic health information. Many hospitals around the world have implemented health information systems.
Government initiatives focus on ensuring interoperability and advancing data sharing to improve healthcare quality and bridge gaps. Thanks to these efforts, the global healthcare interoperability market is expected to grow from $2.9 billion in 2021 to $5.7 billion by 2026, at a CAGR of 13.9%.
In this article, we will define interoperability in healthcare and explore its levels, benefits, standards, and barriers to implementation. We will also share a bit of our healthcare software development experience at IntelliSoft.
Table of Contents
What Is Interoperability In Healthcare?
Interoperability in healthcare refers to the seamless and secure exchange, integration, and use of electronic health data to optimize health outcomes for individuals and populations.
Since implementing the American Recovery and Reinvestment Act (ARRA) in 2009, healthcare providers have shifted from paper-based to electronic health records. ARRA required the electronic exchange of health information technology (HIT) data, a significant development in the healthcare industry in recent years. It has been the primary driving force behind the advancement of interoperability in the industry.
However, the various software programs available in the industry are developed separately, resulting in disjointed communication when used together. Although integrations work to some extent, interoperability aims to provide a complete view of patients despite the differences in technologies used across practices, hospitals, pharmacies, and other healthcare providers.
A survey revealed that 55 percent of CIOs and CMIOs of the top health systems in the United States plan to invest between five to twenty percent more on interoperability in 2023 compared to 2022. Additionally, 43 percent stated that they anticipate spending the same amount in 2023 as they did in 2022.
Why is healthcare interoperability important?
In 2017, about 75% of healthcare providers stored patient data electronically. However, they were unable to easily share important health information such immunization records, allergies, medication lists, and diagnostic imaging. At best, the data could be retrieved, printed or saved on a disc and then shared through manual processes, which was a step in the right direction.
Today, interoperability has become a necessity for several reasons. The following benefits of interoperability in healthcare are the most significant, even though regulatory compliance is not the primary reason for interoperability but rather a means to achieve it.
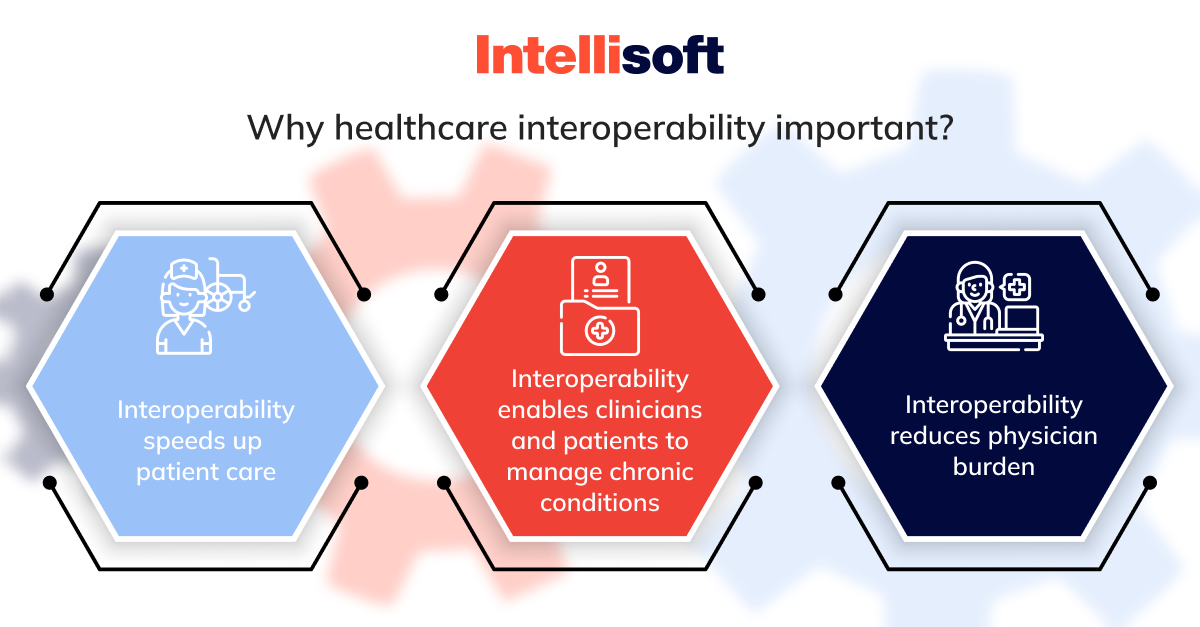
Interoperability speeds up patient care
It is crucial for a healthcare provider, whether they are attending to a medical emergency, treating a patient affected by a natural disaster, or taking over the care of a patient from another provider, to have access to the patient’s medical history, current conditions, ongoing treatments, and any allergies. When healthcare professionals provide medical care to patients, they rely on accurate and trustworthy information. Hence, the information presented at the point of care must be reliable and easily accessible. Moreover, it should be semantically interoperable, meaning different systems and devices can share and understand the data. Additionally, it must be fully auditable, ensuring that any changes made to the data are visible and traceable.
Interoperability enables clinicians and patients to manage chronic conditions
Chronic diseases are a significant cause of concern across the globe, being responsible for a staggering 60% of all deaths worldwide, according to the World Health Organization (WHO). In the United States, the Centers for Disease Control (CDC) reports that a whopping 90% of the nation’s yearly healthcare spending is dedicated to individuals with chronic and mental health conditions. However, the CDC also highlights that effective interventions can be implemented to improve the quality and length of life for those living with chronic diseases.
For instance, diabetes requires regular monitoring by specialists, tracking A1C levels, and adherence to a healthy diet and exercise regime. Successfully managing this chronic condition necessitates a team approach, with all care team members, including the payer organization, having access to vital medical and patient-generated data. To be valuable in population health analytics, patient data needs to be dependable and tailored for clinical outcomes.
Interoperability reduces physician burden
Have you ever had to wait for medical care because of prior authorization or medical necessity requirements? Many healthcare organizations face difficulties in sharing information with payers. Providing the necessary documentation and communicating with payers is a significant challenge for providers. To address this problem, the Department of Health and Human Services (HHS) is prioritizing the promotion of data sharing between payers and providers, particularly with prior authorization. Recent legislation by both CMS and the ONC has supported this goal, and the HL7 accelerator group, DaVinci, is working on developing implementation guides based on the HL7 FHIR standard to reduce the burden on physicians in the pre-authorization workflow.
To promote healthcare data interoperability, HHS has decided to enforce penalties for information blocking on health IT entities starting September 1, 2023. These penalties can be as high as $1 million per violation for severe breaches.
Health information exchanges and interoperability
In today’s world, people expect quick and uninterrupted access to their health records. Healthcare organizations increasingly turn to Health Information Exchanges (HIEs) to meet this demand. These specialized networks rely on interoperable systems to share electronic health information securely and seamlessly.
While adopting Electronic Health Records (EHRs) was a significant first step in building HIEs, multiple challenges still need to be addressed to attain the level of interoperability required for HIEs to deliver their full benefits. Challenges of interoperability in healthcare include:
- Lack of standardization. As the demand for data exchange and big data interoperability in healthcare increases, standard record formats such as FHIR and HL7 are becoming more prevalent. However, many providers and healthcare systems still rely on customized EHR systems, which often pose challenges in converting data into a standard format. As a result, sharing information with other healthcare organizations can be difficult.
- Security. The healthcare industry faces the complex task of striking a balance between making health information easily accessible to those who need it while also ensuring the security and privacy of sensitive patient data. Unfortunately, this challenge is further exacerbated by the rising number of cyber attacks targeting healthcare systems, adding a layer of complexity to an already difficult task.
- Consent. Digital health systems have brought about a revolution in the way healthcare providers manage patient information. However, using such systems also poses a challenge regarding ensuring patient privacy. One of the biggest issues faced by healthcare organizations is determining when patient consent is required for sharing health information and what level of consent is appropriate. The lack of clarity in this regard often results in organizations being overly cautious and withholding information that could be crucial to providing quality care.
- Professional burdens. With the introduction of new recordkeeping tools, the need arises for people to familiarize themselves with the latest systems. However, healthcare professionals can often be apprehensive about adopting new technologies, especially regarding Electronic Health Record (EHR) systems. This is because these systems are primarily designed to support administrative and billing workflows, which may not always align with the needs of clinicians. As a result, it becomes crucial to ensure that new EHR systems are designed with the needs of healthcare professionals in mind so that they can be seamlessly integrated into their daily workflows.
Interoperability challenges in healthcare are not impossible to overcome. Thanks to advancements in cloud computing, particularly hybrid cloud, organizations can do so more efficiently. By leveraging cloud environments, clinicians can create data pipelines that standardize data to a widely accepted industry format like FHIR and provide secure access to key stakeholders such as payers, providers, or patients.
What are the Examples of Interoperability in Healthcare?
The healthcare industry has grown significantly in adopting interoperability standards in recent years. Interoperability refers to the ability of various healthcare systems and applications to communicate and exchange data seamlessly. It has led to integrating complex healthcare systems, improving patient care, data sharing, and public health management. Some prominent interoperability in healthcare examples include the following:
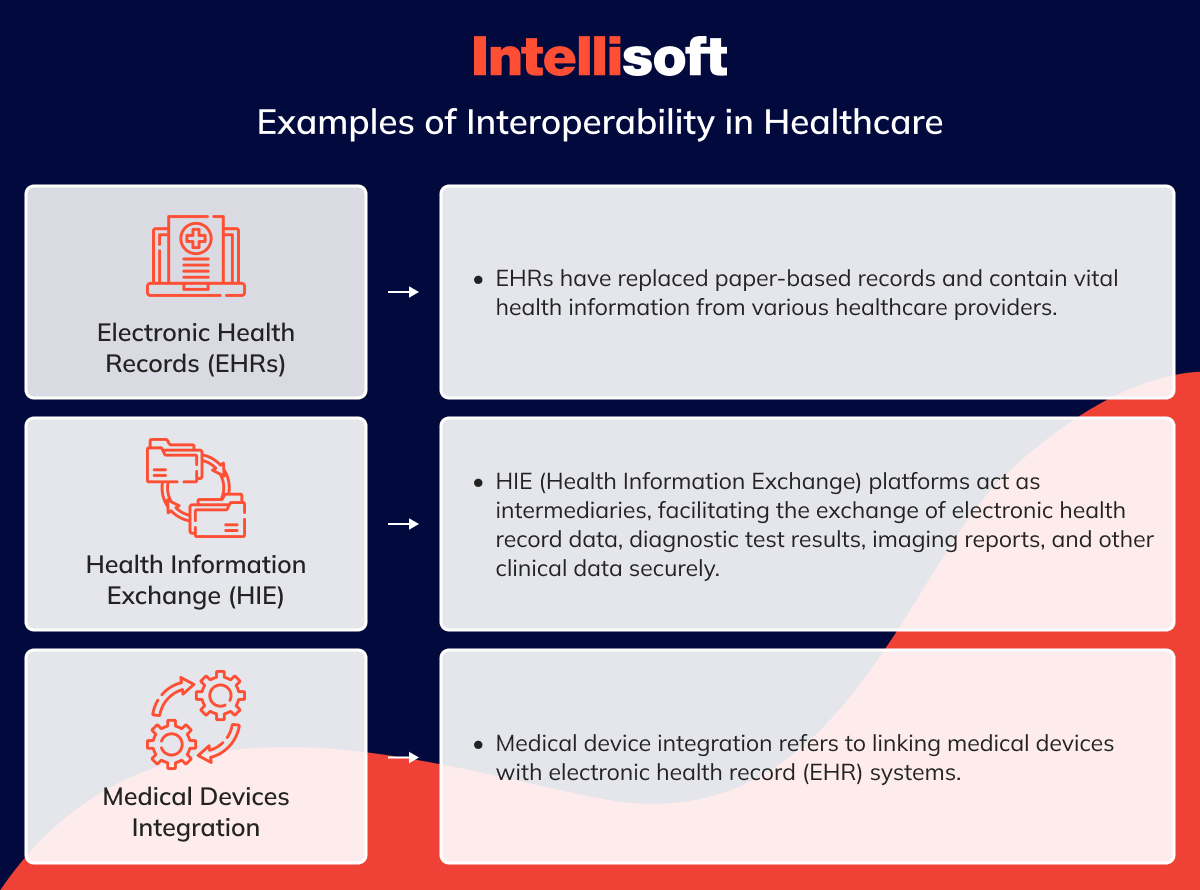
Electronic Health Records (EHRs)
Electronic Health Records (EHRs) are increasingly replacing traditional paper-based records, offering a comprehensive digital version of patients’ medical charts. EHRs contain vital health information from numerous healthcare providers and facilities, making them one of the most significant applications of interoperability in the healthcare industry.
Interoperability allows for seamless sharing of EHR data between various healthcare systems, ensuring authorized providers can access critical patient information irrespective of location. This approach facilitates collaboration among healthcare providers and enables them to make informed decisions about patients’ health, ultimately improving the quality of care they receive.
Health Information Exchange (HIE)
Health Information Exchange (HIE) is a powerful tool for healthcare organizations and providers to exchange critical health information securely. HIE platforms act as intermediaries, facilitating the exchange of electronic health record (EHR) data, diagnostic test results, imaging reports, and other relevant clinical data in a standardized and secure manner.
HIE platforms play a crucial role in revolutionizing healthcare delivery by enabling this interconnected data exchange network. They promote collaboration between healthcare providers and improve data-driven decision-making, ultimately leading to better patient outcomes. HIE platforms have become an essential application of interoperability in healthcare, providing a more efficient and effective way to exchange patient information that can lead to better care coordination and ultimately improve patient outcomes.
Medical Devices Integration
Medical device integration refers to linking medical devices with electronic health record (EHR) systems. When medical devices are interoperable, they can communicate with EHRs, allowing the automatic exchange of patient data, real-time monitoring, and streamlined documentation. This integration and interoperability in healthcare improves patient safety, helps healthcare professionals make better decisions, and increases the overall efficiency of healthcare delivery.
Levels of Healthcare Interoperability
Interoperability in healthcare is categorized into four levels as defined by informatics experts and the Healthcare Information and Management Systems Society (HIMSS). While some of these levels are attainable with the existing IT systems and architecture in healthcare, others require further innovation and development in patient-centered technology. Let’s look at the four types of interoperability in healthcare.
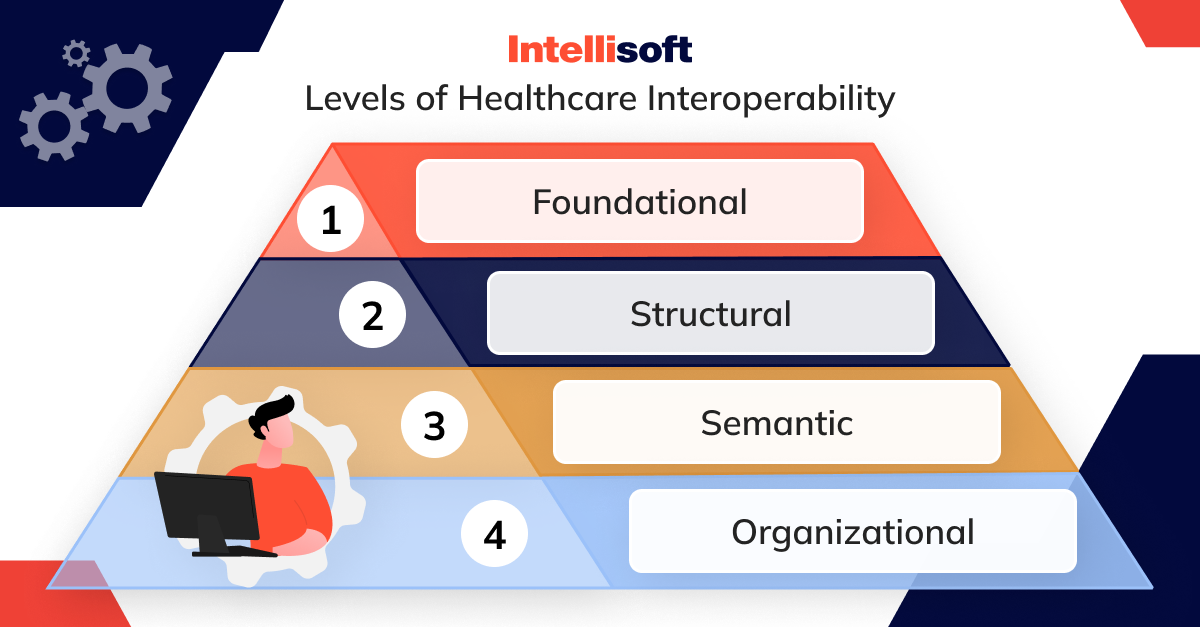
Foundational
Interoperability is the ability of different systems and devices to communicate and exchange data. At the most basic level of interoperability, the superficial transport level, data is transferred securely between systems or devices without any interpretation or transformation into a specific format. For example, a nurse may access a laboratory’s portal to download a PDF file containing a patient’s laboratory results and manually enter the data into the patient’s health record. This data exchange process may seem simple, but it is an essential element of effective healthcare data management, allowing different systems and devices to work together seamlessly and efficiently.
Structural
Structural interoperability is a crucial process that enables multiple systems or devices to communicate with each other seamlessly. This involves standardizing all the data to a particular format so that the receiving system can easily interpret the data fields. This approach ensures that records are consistent, centralized, and easily transferred between different systems. The data is organized in a specific order, following standards such as FHIR and HL7, which provide a consistent format for data exchange. This data standardization is essential for healthcare providers, as it allows them to access and share vital patient information efficiently, leading to better healthcare outcomes.
Semantic
Interoperability involves exchanging data between different systems with varying structures. For instance, medical imaging systems have different DICOM and non-DICOM formats for images. Semantic interoperability in healthcare aims to transfer images from one system to another, regardless of the original format or source, and interpret them into the new system. However, determining which data to collect and transfer can prove challenging since systems present data differently. Therefore, some experts believe using artificial intelligence will be necessary to achieve full semantic interoperability.
Organizational
Organizational interoperability refers to the ability of different organizations to exchange data seamlessly despite having different requirements, regulations, and goals. Achieving this level of interoperability requires policy and governance innovations and technological innovations to ensure that consent, security, and workflows are integrated and move smoothly between different groups. Although some experts argue that semantic interoperability is the highest level of interoperability, others believe that organizational interoperability holds the utmost importance.
Related articles:
- Inside Out: Exploring the World of Diagnostic Medical Imaging Software
- Predictive Analytics in Healthcare: How To Implement In Your Organization
- How Artificial Intelligence Innovates the Healthcare Industry
- Leveraging Data Analytics: A Guide to Revolutionizing the Pharmaceutical Industry
- Prescription Management Software: The Future of Pharmacy
Types of Data Involved
Healthcare interoperability in the United States is a crucial process that enables multiple healthcare systems and stakeholders to communicate and collaborate seamlessly by exchanging and integrating different data types. Clinical, administrative, and financial data are the primary data types involved in healthcare interoperability. Here’s a brief description of each type, along with some examples:
Clinical Data
Clinical data is an essential aspect of healthcare that refers to a wide range of information about a patient’s health status and medical history. It includes detailed data collected during clinical encounters, such as doctor consultations, laboratory test results, imaging reports, medication prescriptions, allergies, and vital signs. This data is critical for physicians to make informed decisions regarding a patient’s diagnosis, treatment, and healthcare outcomes. For instance, when a patient is referred to a specialist, the referring physician can share relevant clinical data, such as medical history, test results, and treatment plans, to ensure continuity of care. This data is also used to facilitate research and analysis of healthcare outcomes and trends in patient care.
Administrative Data
Administrative data is crucial in managing various non-clinical aspects of the healthcare industry, such as resource allocation, billing, and healthcare operations. This data comprises vital information such as patient demographics, insurance details, appointment schedules, billing codes, and claims data collected when a patient visits a healthcare facility. The primary purpose of collecting administrative data is registering patients, verifying their insurance coverage, and effectively managing the billing and reimbursement processes. This information facilitates the smooth functioning of healthcare facilities, ensuring patients receive the medical attention they require without unnecessary delays or complications.
Financial Data
Financial data in healthcare is a crucial aspect that deals with the monetary transactions involved in medical services. This information entails various financial factors, such as healthcare costs, payments, and reimbursements. It encompasses the pricing of healthcare services, insurance claims, and payment transactions. For instance, when a healthcare provider submits a claim to an insurance company, financial data is shared to verify the services provided, determine coverage, and process payment. Financial data in healthcare plays a vital role in ensuring that all monetary transactions are handled accurately and efficiently, making it an indispensable aspect of the healthcare system.
Interoperability Standards and Frameworks
In medicine, data exchange is governed by various standards, just like any other industry. Interoperability standards are a set of common rules that enable the transfer and interpretation of patient data across different systems.
Standard development organizations (SDOs) are responsible for developing, updating, and maintaining interoperability standards. Creating such standards is a complex process that usually involves collaboration with healthcare experts and stakeholders who will ultimately adopt the standard.
HIMSS has classified all the currently available interoperability standards into different types.
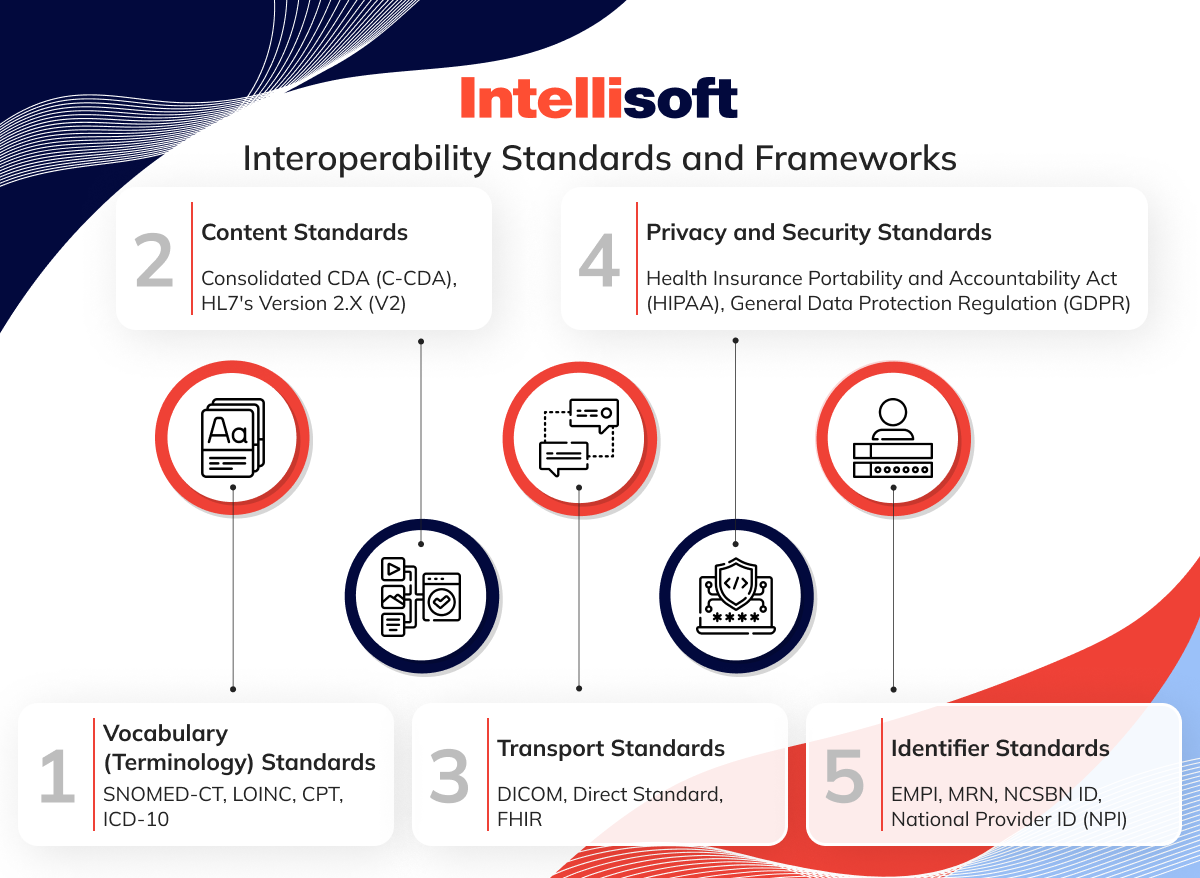
Vocabulary (Terminology) Standards
The vocabulary standards ensure that medical concepts are interpreted without ambiguity by sending and receiving machines. These standards use structured codes and terminologies to represent health and clinical concepts such as diseases, diagnosis, medications, etc. As a result, all systems will interpret the health data accurately.
Several popular vocabulary standards include SNOMED-CT for clinical terms, LOINC for laboratory and clinical tests, CPT for billing procedures, and ICD-10 for diseases and injuries.
Content Standards
Interoperability standards aim to unify the structure and location of content in shared documents and specify common sets of data to be used in specific messages.
Consolidated CDA (C-CDA) and HL7’s Version 2.x (V2) are the most commonly used content standards. These standards streamline communication between providers and patients by specifying the semantics and organization of exchanged documents.
Transport Standards
The standards that govern electronic message format, architecture, templates, and user interfaces play a crucial role in ensuring seamless data sharing between different systems. A message refers to a distinct unit of information transmitted from one software to another. These standards define the rules and regulations that must be followed to ensure that messages are correctly formatted and can be interpreted by the recipient system, thereby enabling efficient communication between different entities.
Transport standards facilitate interoperability by using push and pull approaches to exchange health data. Examples of such standards include DICOM, intended for transmitting medical images; Direct Standard, intended to carry C-CDA formatted data; and FHIR, which uses RESTful APIs to share documents in XML, JSON, or RDF formats.
Privacy and Security Standards
Interoperability standards have been developed to ensure the safety and security of patient health data. These standards define how patient health data can be collected, accessed, processed, and disclosed.
Two significant laws aim to protect the privacy and security of patient health information. The Health Insurance Portability and Accountability Act (HIPAA) sets stringent standards for safeguarding health information privacy in the United States. HIPAA ensures that sensitive healthcare data is protected from unauthorized access while giving patients control over their personal health information.
In the European Union, the General Data Protection Regulation (GDPR) sets forth comprehensive privacy and security regulations for storing and processing information across all industries, including healthcare. GDPR necessitates that healthcare providers implement security measures, such as encryption and access controls, to protect patient data. It also provides patients with a range of rights to control how their personal health data is accessed and used.
Identifier Standards
These standards help to identify healthcare providers and patients across various platforms. Examples of these standards include EMPI, which healthcare organizations use to maintain patient records; MRN, which hospitals use to keep a patient’s history throughout their stay; and NCSBN ID, which serves to verify nurse licenses; and National Provider ID (NPI), which represents a 10-digit identifier for healthcare providers.
The Challenges of Interoperability In Healthcare
A clinic holds up to 12% of duplicated medical records. In addition, up to 33% of records contain incorrect patient data, which is a major challenge for EHR interoperability.
According to a report by EHRIntelligence, 88% of hospitals can electronically exchange clinical data. However, other healthcare organizations face challenges that prevent them from sharing medical data or restrict them from exchanging only basic-level information. Let’s look at the critical challenges of interoperability in healthcare and the adoption barriers for healthcare interoperability.
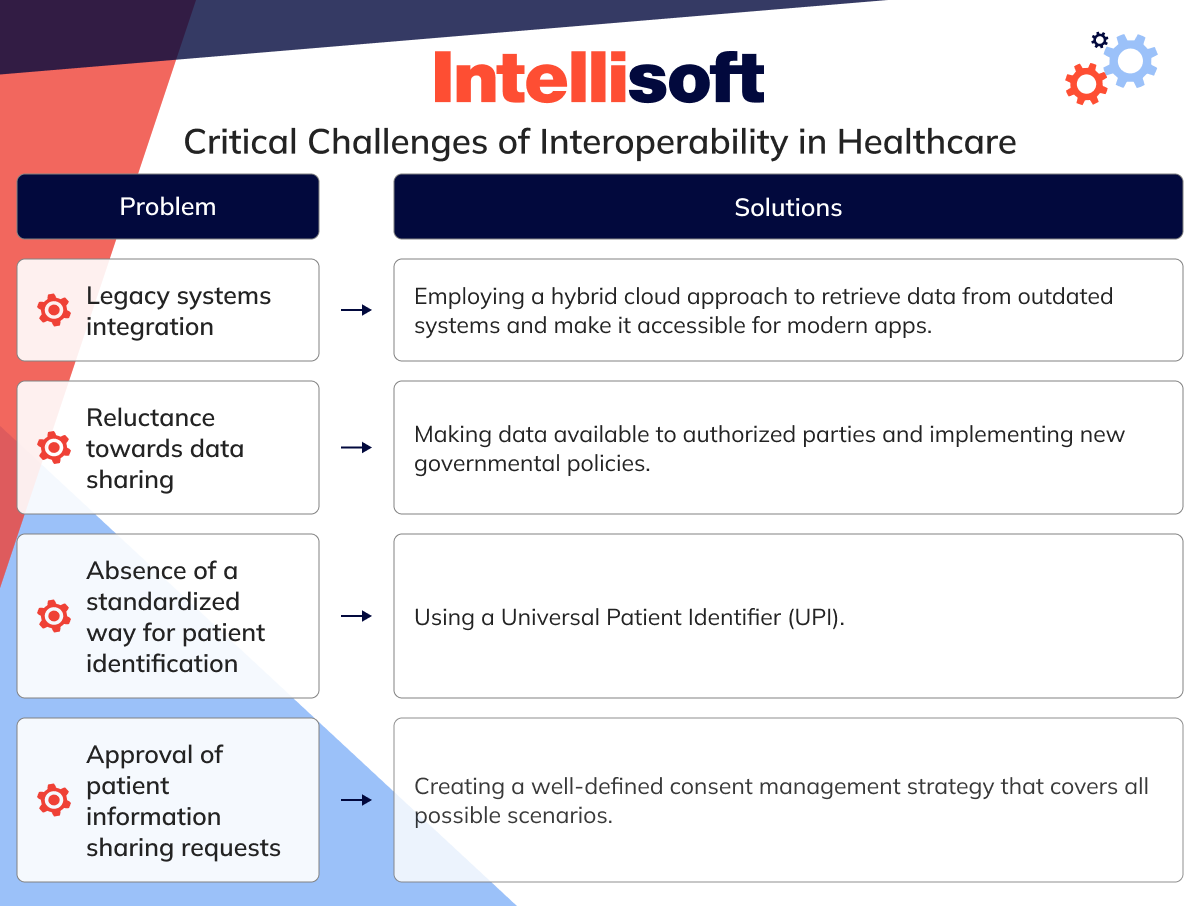
Legacy systems integration
Legacy systems are still widely used in the healthcare industry. According to reports, as of January 2020, Microsoft no longer supports 70% of Windows-based medical legacy devices. Many of these systems were designed in an era with limited network connectivity and lacked modern security features, making them difficult to maintain. To comply with the existing interoperability standards, it is necessary to modernize these systems.
As a temporary measure, healthcare organizations might employ a hybrid cloud approach to retrieve data from outdated systems, making it accessible for modern apps. Additionally, some healthcare interoperability standards are better suited to legacy system integration and interoperability in healthcare. For instance, FHIR provides well-documented mappings for legacy standards.
Reluctance towards data sharing
Certain players are hesitant to share their patient data in the healthcare industry. Hospitals, for instance, often compete with urgent care clinics for patients. Therefore, hospitals are not inclined to oblige when such a clinic requests patient data. This situation arises when sharing health data for research since universities compete for funding.
To achieve data interoperability in healthcare systems, healthcare facilities must change their mindset and make data available to authorized parties, hoping they will do the same in return. New governmental policies are also expected to be implemented to support health data sharing. For instance, Pew Charitable Trusts has urged the Biden administration to address data exchange practices.
Absence of a standardized way for patient identification
Medical facilities often use a combination of a patient’s name, birth date, and social security number to identify them. However, this combination has no standardized format; not all clinics use the same method to identify their patients. This uniformity in patient identification can lead to a lack of interoperability in healthcare, as there is no widely accepted way to refer to a patient.
A possible solution to the medical identification problem is the Universal Patient Identifier (UPI). UPI is a unique identification number that is only used for healthcare data, meaning anyone who has it cannot access someone’s financial information.
Approval of patient information sharing requests
Healthcare organizations prioritize ensuring the safety and security of patient data. To achieve this goal, it is crucial to have a well-regulated process for validating and approving requests.
To maintain patient privacy and comply with legal requirements, it is crucial to have a well-defined consent management strategy. This strategy must cover all possible scenarios where consent is required for a patient, including situations where a responsible person, such as a parent or legal guardian, provides consent on behalf of the patient.
5 Tips For Improving Data Interoperability In Healthcare
If you are working for a healthcare organization and striving to improve health data interoperability, you may wonder how to improve interoperability in healthcare. These tips are based on industry best practices and can help streamline data sharing between different healthcare systems, improve patient care, and boost operational efficiency.
Ensure anonymity
Protecting patient privacy is of utmost priority for healthcare organizations. Therefore, ensuring that no unauthorized third party can access patient information without full anonymization is crucial. This approach includes external vendors who assist in developing and maintaining applications, researchers who analyze data for disease studies, and anyone not directly involved in a patient’s care.
Establish a reliable patient consent process
To improve the exchange and usability of healthcare data, it is crucial to establish a clear and transparent consent protocol that will encourage patients to participate actively. This protocol should include policies that prevent unauthorized access and transmission of patient data and ensure that all data sharing is conducted in line with the patient’s explicit consent. If you want to encourage patients to consent, explain how their data may be used to develop innovative treatments and potentially save lives.
Moreover, partnering with reputable organizations with a history of advocating for patient rights can help build trust and encourage participation. By prioritizing transparency, patient empowerment, and collaboration, the outsourcing software development team can work towards creating a more streamlined and effective healthcare system that benefits patients, healthcare providers, and researchers alike.
Manage IT integration
When creating a data ecosystem, you should consider two key things:
A data layer that provides APIs for your partners to integrate their data repositories. Ensure that this layer complies with the most common healthcare interoperability standards.
A data management approach that guarantees uniformity and confidentiality. Furthermore, once your data is systematically arranged, you can investigate additional applications for healthcare data utilization.
Use health information exchange (HIE) services
Health Information Exchange (HIE) is a tool that helps to transfer clinical data among various health information systems while keeping its meaning intact. If the service is available to you, you can connect to it. For instance, New York offers its own HIE tool called the Statewide Health Information Network for New York (SHIN-NY), which connects all the city hospitals and many independent practitioners. SHIN-NY is constantly expanding and improving patient care.
Move your data to the cloud
Organizations are increasingly relying on cloud-based interoperability solutions in healthcare. According to recent studies, 82% of small practices located in urban areas have already adopted Electronic Health Record (EHR) systems based on cloud technology. Furthermore, 81% of these practices have reported high satisfaction levels with the system. Cloud-based solutions offer many benefits to the healthcare sector, such as improved data interoperability.
Final Thoughts
Healthcare is a data-driven industry, and modern organizations require seamless and timely access to health records. The ability to share, interpret, and utilize health data is essential to ensure that healthcare providers can achieve smooth data flow across platforms without user intervention. This is where interoperability comes into play. Interoperability in healthcare systems is essential for creating a connected and efficient healthcare ecosystem where data flows seamlessly between different systems and providers.
At IntelliSoft, we understand the significance of interoperability and offer healthcare software development services centered around this transformation. Our services help healthcare organizations to achieve significant cost savings, reduce errors, make timely and balanced decisions, and provide 24/7 real-time access to health records. By adopting interoperability, healthcare providers can unlock the full potential of health data, leading to better patient outcomes and improved healthcare services.
Our client, Daintel, requested the transformation of their MVP into a comprehensive medical information system, enhancing its performance and integrating critical ICU modules. With a focus on interoperability, this system now supports seamless communication and data exchange across different healthcare departments and systems. It includes functionalities such as prescription management, patient health monitoring, and advanced data analytics, facilitating a unified approach to patient care and management.
Our team of developers has extensive experience building interoperability solutions in healthcare and is always ready to consult and help implement technologies in your organization. If you’re interested in our offer, contact us today. Let’s work together towards reaping the benefits of fully interoperable healthcare systems as soon as possible.