One of the main sectors that is changing and growing thanks to digitalization is healthcare. EHR and EMR software helps healthcare practitioners manage healthcare data more efficiently, simplifies the consultation process, and provides a better service for patients. By 2027, the Global Electronic Health Records (EHR) market size is expected to hit $52.98 billion, once again proving that EHR systems are revolutionizing healthcare.
The healthcare sector is now heavily relying on e-documents, e-prescriptions, and other electronic forms, with traditional documentation becoming outdated and used by fewer and fewer institutions. Nowadays, more than 95% of US hospitals use Electronic Health Record platforms, helping both practitioners and patients improve their experiences at healthcare establishments.
If you have been thinking about developing an EHR system for your healthcare institution, it’s time to act. With so many institutions already relying on software tools for optimized healthcare operations, going digital is the only way to stay competitive and offer your patients high-quality service. Fortunately, at IntelliSoft, we have been assisting our clients from the healthcare sector for more than 15 years, and we know exactly how to facilitate seamless data sharing and improve medical care in your organization. We can’t keep this knowledge a secret, so let’s embark on this journey together and answer your question “How much do EHR systems cost?”.
Table of Contents
What is an Electronic Health Record System
Before answering the question “How much does an EHR system cost?”, let’s talk about what an EHR is. An Electronic Health Record system, short for Electronic Health Record, serves as a robust software repository housing vital patient health data. This system includes comprehensive information such as:
- Medical history
- Lab data
- Test results
- Vaccination details
- Allergies
- Progress notes
- Medications
- Insurance information
It’s crucial to distinguish Electronic Health Record systems from EMR software. While they can be used interchangeably, there is still a significant difference between the two. EMR, or Electronic Medical Record, functions as a digitized version of a patient’s chart localized within a specific clinic. It encapsulates the medical history pertinent to a particular practice.
In contrast, EHRs are designed with broader functionality, intended for seamless sharing of health information among various entities, including laboratories and other healthcare providers. EMRs can’t share any information outside of the clinic.
Types of Electronic Health Record Systems
There exist two main types of EHR systems; physically hosted and remotely-hosted. If you want to build your own EHR, understanding the difference between these two types is crucial.
Physically Hosted Electronic Health Record Systems
Physically hosted EHR systems involve the installation and operation of the software on servers that are physically present within the healthcare facility. This setup provides a sense of control and autonomy, allowing organizations to manage and maintain their server infrastructure. It’s an ideal choice for those prioritizing in-house control over data and system management.
Remotely Hosted EHR Systems
On the other hand, remotely hosted Electronic Health Record systems, often referred to as cloud-based solutions, leverage external servers provided by third-party vendors. These systems operate via the Internet, enabling healthcare organizations to access and manage patient data without the need for extensive on-site server infrastructure. Remotely-hosted options often boast scalability, flexibility, and the advantage of offloading maintenance responsibilities to experienced service providers.
Benefits of EHR Systems
EHR platforms offer numerous advantages for all stakeholders involved; businesses, hospitals, and patients. It’s critical to know how you and your patients can benefit from a custom EHR before building it, so let’s dive into the main benefits of EHR systems for physicians and patients.
Benefits of EHR for Physicians
Electronic Health Record (EHR) systems have a multitude of advantages for physicians, revolutionizing the way healthcare information is accessed, managed, and utilized. Here are the key benefits of EHR system for medical practitioners:
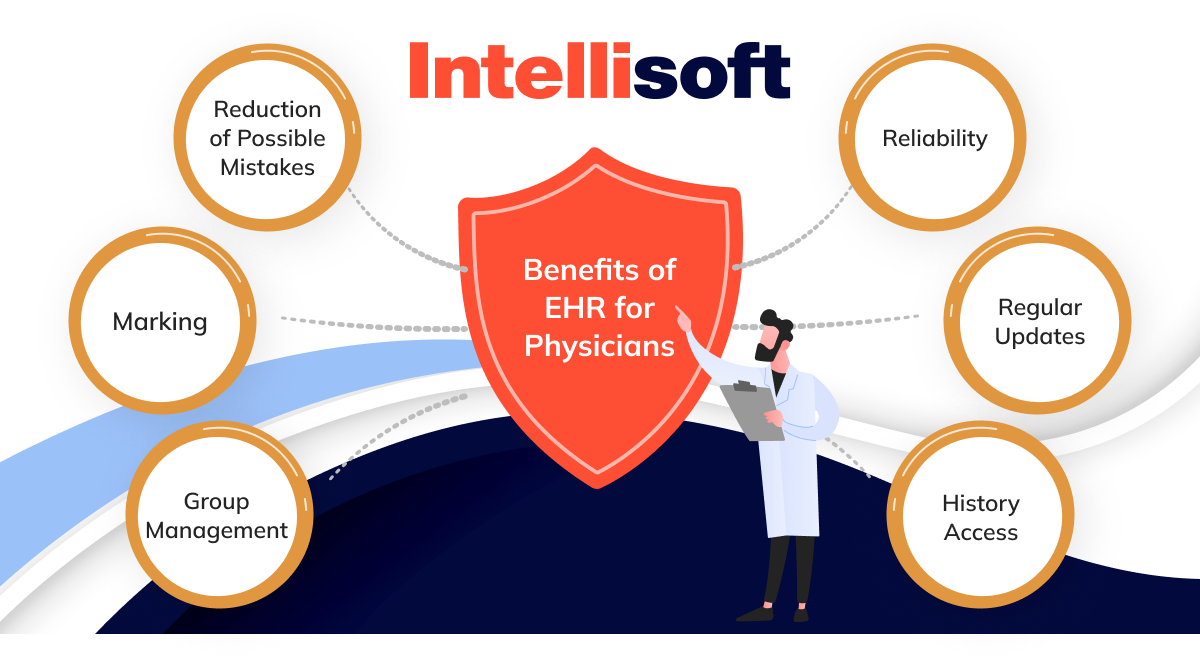
- Reliability. EHR systems ensure the reliability of patient data by centralizing information in a secure and easily accessible digital format. Physicians can rely on accurate, up-to-date data for informed decision-making, enhancing the overall quality of patient care.
- Regular Updates. Staying abreast of the latest medical advancements and regulatory changes is essential. One of the main benefits of EHR system is that is provides practitioners regular updates, ensuring that the software remains aligned with evolving healthcare standards and practices.
- History Access. Accessing a patient’s comprehensive medical history at a glance is a game-changer. EHR systems consolidate historical data, empowering physicians to make well-informed diagnoses and treatment decisions based on a thorough understanding of a patient’s health journey.
- Reduction of Possible Mistakes. The transition from paper-based records to EHR systems significantly reduces the likelihood of errors. Improved legibility, standardized documentation, and built-in error-checking mechanisms contribute to a safer healthcare environment with fewer potential mistakes.
- Marking. EHR systems facilitate efficient marking of critical information within patient records. Physicians can highlight important details, track changes, and annotate records, ensuring that vital information is readily accessible during subsequent visits or in collaborative settings.
- Group Management. Collaboration among healthcare professionals is streamlined through Electronic Health Record systems. Physicians can seamlessly manage and share patient information within a group, fostering effective communication and coordinated care.
Benefits of EHR for Patients
Electronic Health Record (EHR) systems also provide a ton of benefits for patients, bringing forth a range of benefits of EHR system designed to enhance the quality, accessibility, and convenience of medical care:

- Timely Care
EHR systems enable healthcare providers to access comprehensive patient information swiftly, leading to more timely and informed care. Patients can experience quicker diagnoses, personalized treatment plans, and expedited healthcare services. - Integrated Communication
Seamless communication among healthcare professionals is facilitated by Electronic Health Record systems, ensuring that patients’ medical information is shared efficiently between providers. This integrated approach fosters collaborative care, leading to more cohesive and effective treatment strategies. - Appointment Management
Patients reap the benefits of streamlined appointment scheduling and management through EHR systems. Automated appointment reminders, real-time availability updates, and easy rescheduling options contribute to a more organized and patient-centric healthcare experience. - Medical Data Tracking
EHR systems empower patients to actively participate in their healthcare journey by providing access to their medical data. Tracking health metrics, test results, and treatment plans becomes more accessible, enabling individuals to make informed decisions about their well-being. - Card Scanning
The integration of card scanning features in Electronic Health Record systems simplifies the process of updating personal and insurance information. Patients can effortlessly provide accurate details, reducing administrative burdens and ensuring that records are always current. - Reminders
Patients benefit from automated reminders for medication schedules, upcoming appointments, and preventive health measures. EHR systems contribute to improved adherence to treatment plans, fostering better health outcomes. - Cloud Hosting
The adoption of cloud hosting in EHR systems ensures secure and accessible storage of patient data. This not only enhances data security, but also allows patients and authorized caregivers to access health information from anywhere, promoting continuity of care.
SaaS vs. Custom Electronic Health Record System
The decision between opting for a Software as a Service (SaaS) solution and investing in a custom-built Electronic Health Record system is pivotal. While SaaS solutions offer convenience, developing a custom
EHR solution holds a spectrum of long-term benefits that transcend the immediate ease of implementation.
Benefits of Custom EHR Development

- Tailored to Your Unique Needs. A custom EHR is crafted to align precisely with the specific workflows, processes, and requirements of your healthcare facility. This tailored approach ensures optimal efficiency and relevance, addressing the unique challenges of your practice.
- Scalability and Flexibility. As your healthcare facility evolves, so can your custom EHR system. The scalability and flexibility inherent in a bespoke solution allow seamless adaptations and integrations, ensuring that your technology remains in sync with the dynamic landscape of healthcare.
- Enhanced Security and Compliance. Custom EHRs offer a heightened level of data security as they can be designed with your facility’s specific compliance requirements in mind. This proactive approach to security minimizes vulnerabilities and ensures compliance with industry regulations.
- Optimal User Experience. Tailoring the user interface and experience to the preferences of your healthcare professionals enhances overall usability. This results in a more intuitive system, reducing training time and increasing user satisfaction.
- Long-Term Cost Efficiency. While the upfront investment for custom EHR development may seem higher, the long-term cost efficiency becomes evident. Custom solutions eliminate the need for ongoing licensing fees and reduce the risk of unexpected expenses associated with adapting pre-built systems to meet your evolving needs.
Common Hidden Fees for SaaS EHR Software
When you wonder “How much does an EHR system cost?” and outline your budget for a SaaS EHR system, you need to consider possible hidden fees and expenses, such as:

- Implementation and Setup Costs. Cost of EHR implementation can vary widely based on your practice’s complexity and the chosen EMR provider, typically ranging from $5,000 to $20,000.
- Training Expenses. While basic training may be included, advanced or ongoing sessions can cost an additional $1,000 to $5,000 or more, depending on the level of training needed.
- Data Conversion Fees. Ranging from $2,000 to $10,000, these fees depend on data volume and conversion complexity.
- Support and Maintenance. Ongoing fees usually range from $100 to $500 per user per month, potentially totaling $6,000 to $30,000 annually for a small practice.
- Interoperability Costs. Efforts may cost several thousand dollars, particularly if extensive integration work is required.
- Hardware Costs. For in-office solutions requiring hardware, expect costs from $5,000 to $20,000 for servers and related components.
- Add-On Modules and Features. Variable cost of EHR systems, ranging from $100 to $1,000 per user per month, depending on functionality.
- User Licensing Fees. Additional user fees may add $50 to $200 per user per month to expenses.
- Data Storage Fees. Additional storage cost of EHR systems range from $100 to $500 per month based on data volume.
- Upgrades and Customization. Upgrades may cost 10% to 20% of your initial license cost, while customization expenses vary from $5,000 to $20,000.
- Penalties for Early Contract Termination. Termination penalties may range from $2,000 to $10,000, depending on contract terms.
- Third-Party Integration Fees. Integration fees can range from $1,000 to $5,000 per integration.
Essential Features of Custom EHR System
Every custom EHR solution is built according to unique client’s needs and requirements, so the set of features will be different in each software. However, some functionalities are a must for every EHR, and your development team will ensure that they are added to your software solution.
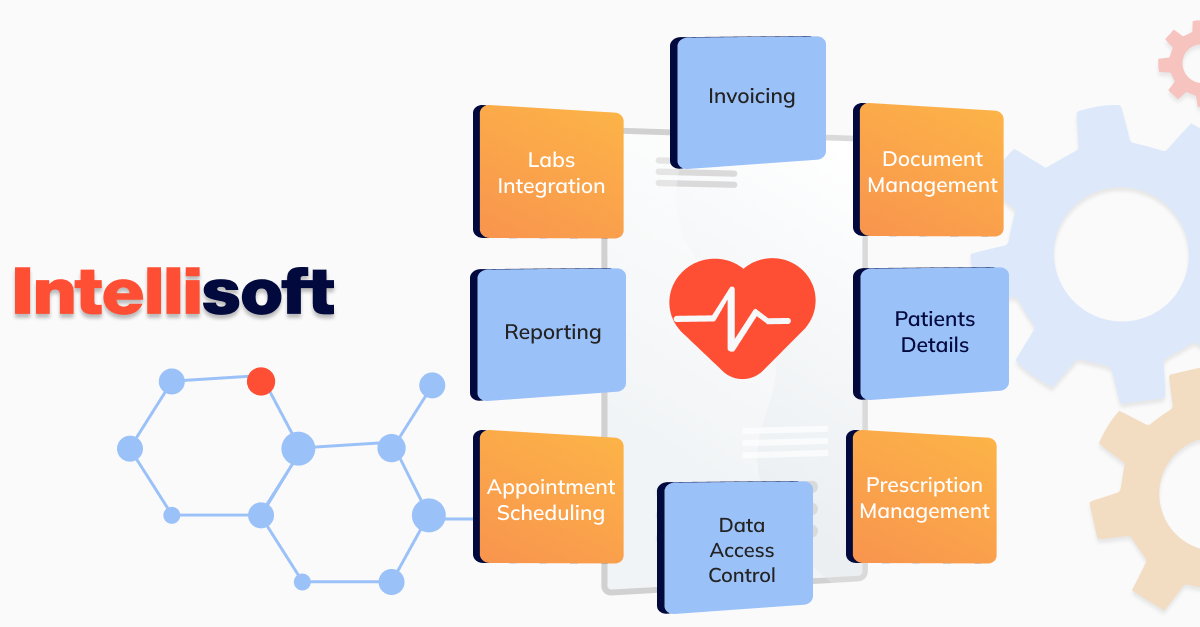
Document management
Your EHR system should primarily help patients receive better care by offering them a convenient way of managing their healthcare documents. Both patients and doctors should be able to upload documentation easily across multiple formats, including DICOM (MRT and CT images), textual, image, etc.
Patients details
All EHR systems should contain patients’ personal data, such as their full name, address, diagnosis, treatment details, test results, prescriptions, and other important information that provides insights into patients’ health.
Prescription management
Leveraging the e-prescribing functionality, physicians can remotely prescribe medications to patients while accessing their medical data to verify drug compatibility. Simultaneously, patients have the capability to monitor their medication history.
Data access control
EHR systems contain sensitive patients’ data, so a high-quality should have all the necessary data access control mechanisms in place. It means that people from different levels should not have access to the same data. For example, a nurse should not have access to the same data as doctors.
Appointment scheduling
The electronic health record software enables patients to schedule real-time appointments with their doctors. Meanwhile, doctors have access to a dashboard displaying appointments alongside patient details.
Reporting
Your custom EHR should have strong reporting features to help practitioners have a complete picture of patient data, treatment, rate of treatment success, and so on. Patients can also make use of this feature and gain insights into how their treatment is going, what time their next appointments are, etc.
Labs integration
Connecting Electronic Health Records (EHR) with test labs ensures rapid data exchange and quicker decision-making. What enhances its efficiency is the direct transmission of test results to applications, enabling easy access for patients and doctors to take prompt action.
Invoicing
All healthcare institutions have to deal with invoices, denials, claims, and payments for treatments, hospitalization, etc. This process has long been too complicated due to relying on paper documentation. With the introduction of EHR systems, invoicing became digital and automated. Nowadays, all EHR systems have an invoicing feature, allowing patients to pay for everything using software.
How Much Do EHR Systems Cost
It’s not easy to answer the question “How much does it cost to implement an EHR system?” without talking about factors that affect the cost. The cost of developing a bespoke EHR solution can differ depending on multiple factors such as your requirements, features you want to implement, the development team and their location, integration with third-party systems, etc. In our experience, the final cost of EHR implementation is usually between $50,000 and $500,000. While it’s not possible to determine a price, you should learn about the factors that can influence it. Here’s an EHR implementation cost breakdown:
- Features complexity and number
The complexity and quantity of features embedded within the EHR system play a pivotal role in determining the average cost of hospital EHR implementation. Advanced functionalities, intricate workflows, and an extensive feature set contribute to increased development efforts, consequently impacting the budget. - Scalability and customization
A scalable EHR system ensures adaptability to evolving needs and growth. The development of a scalable architecture demands meticulous planning and execution, adding to overall EHR pricing. Additionally, customization tailored to the specific requirements of the healthcare facility contributes to the development complexity and cost. - Third-party system integration
The integration of third-party systems, such as laboratory systems or billing platforms, introduces a layer of complexity. The level of integration, seamless data exchange, and compatibility with diverse external systems all influence the development effort and, subsequently, the EHR pricing. - UI/UX design
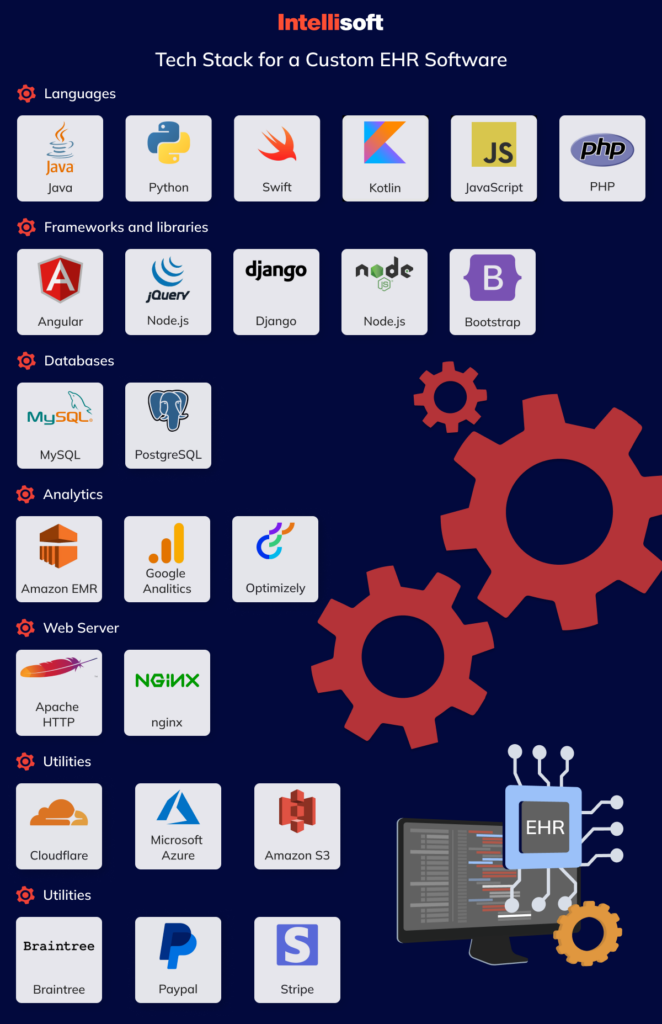
The user interface (UI) and user experience (UX) design are critical components that impact how seamlessly healthcare professionals interact with the EHR system. A well-designed, intuitive interface necessitates a thoughtful investment in design expertise, potentially influencing the average cost of hospital EHR implementation. - Tech stack
The technology stack chosen for EHR development, encompassing programming languages, frameworks, and databases, directly shapes the project’s complexity and EHR pricing. Opting for cutting-edge or specialized technologies may contribute to a higher initial investment. - Compliance
Ensuring compliance with healthcare regulations and industry standards is paramount. The development of robust compliance features, including data security and privacy measures, requires additional resources, impacting the complexity and cost of EHR implementation (hospital and other healthcare institutions).
Here’s how much time various factors take during the development process:
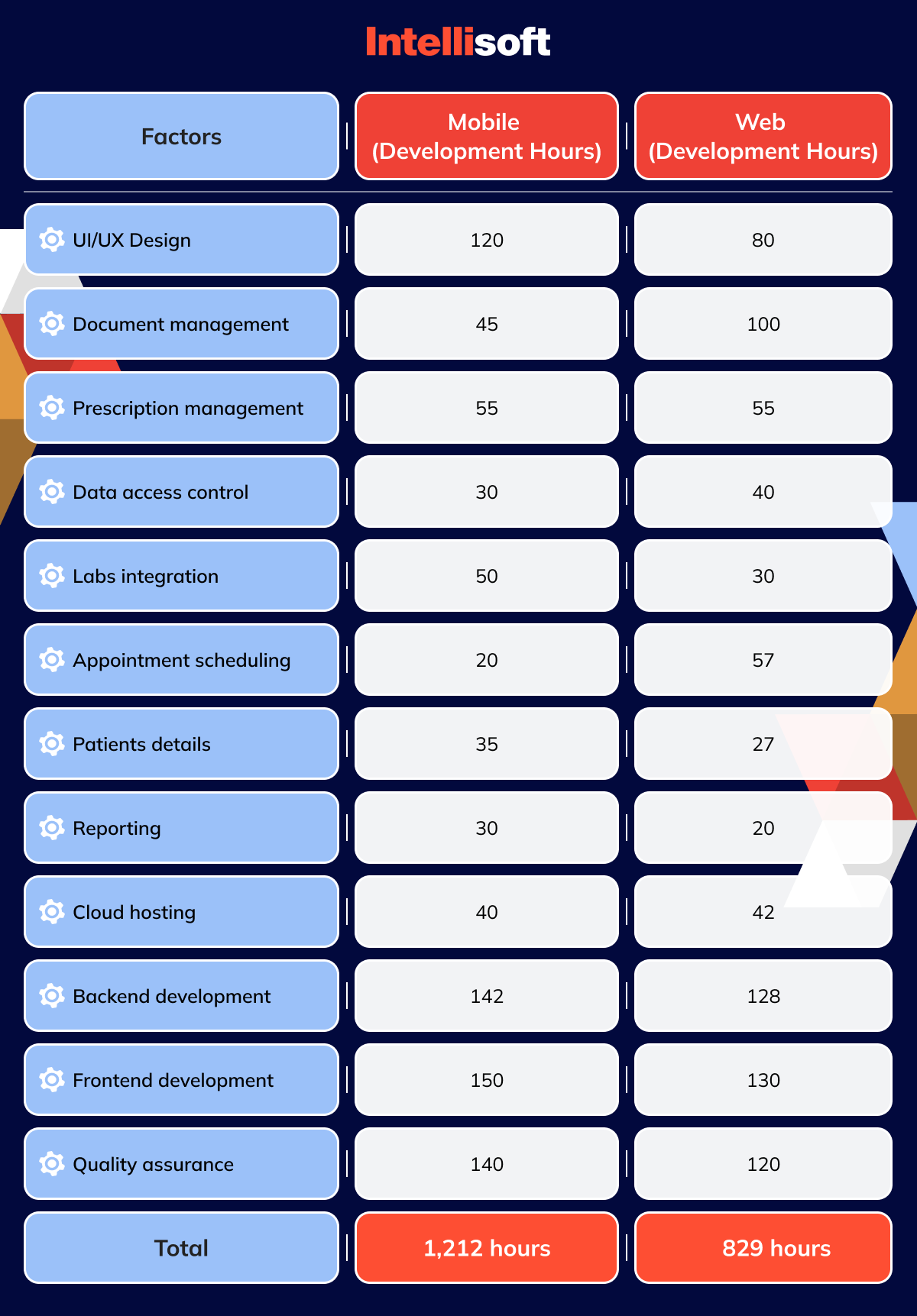
How much does it cost to implement an EHR system, then? When translating these hours into the average rates charged by a healthcare software development company, ranging from $50 to $80 per hour, the projected costs fall within the following numbers:
- Web-based EHR cost: $41,450 – $66,320
- Mobile EHR platform: $60,600 – $96,960
It’s crucial to acknowledge that these development hours and associated costs pertain specifically to the Minimum Viable Product (MVP) version of an Electronic Health Record (EHR). For the advanced version, a distinct and upgraded set of numbers will apply.
Here are the features included in an advanced version of an EHR:
- Auto-scheduling
This feature could be your key to staying competitive and standing out in the market. This feature will allow your software solution to keep track of doctor’s appointments and automatically handle the next. - Vendor selection
All healthcare institutions work with several vendors, all having different locations, costs, and so on. Usually, the number of vendors makes it challenging to track them all and filter manually. An EHR can help automate the process by adding a filtering and tracking feature, making it easier for clinicians to select vendors. - Customer Relationship Management
The success of an Electronic Health Record (EHR) system hinges on patient adoption, and to facilitate this, integrating a Customer Relationship Management (CRM) module is pivotal. This CRM should include features such as real-time chat, report viewing, complaint submission, newsletters, and push notifications. By incorporating these elements, healthcare providers enhance patient engagement, promote effective communication, and encourage active patient participation in their healthcare journey. - Next-generation technology integration
Nowadays, healthcare organizations are not afraid of experimenting with advanced technology such as AI and ML, Blockchain, etc. These technologies can help make the systems even more secure, effective, and innovative.
These represent just a few instances of the factors or enhancements that can elevate your EHR system from its Minimum Viable Product (MVP) version to an advanced iteration. The associated EHR implementation cost breakdown considerations for these upgrades are as follows:
- MVP-level EHR cost range: $41,000 to $97,000
- Advanced-level EHR cost range: $50,000 to $120,000
Related readings:
- Automation in the Industry of Healthcare: Main Benefits for Business
- Predictive Analytics in Healthcare: How To Implement In Your Organization
- Hospital App Development: Innovate, Integrate, and Provide Better Care
- What Technologies Are Driving the Health Protection System?
- Technological Trends in Healthcare in 2023
Steps to Build an EHR System
Once you have learned what is the cost of an EHR system, let’s move on to what it takes to develop it. Building an EHR system from scratch is a complicated endeavor, as the development team should have prior experience and the technical skills required for such development. In most cases, healthcare institutions choose to opt for third-party development assistance, reaching out to software development vendors.
Hire a Team
First of all, you need to select and hire a development team you are going to work with. The global talent pool is exceptionally rich nowadays, offering you teams from all over the globe with skills and knowledge you can benefit from. But, the choice will not be an easy one, as you should thoroughly examine candidates’ websites, expertise, successful cases, and make sure that they are a perfect fit for your project. When hiring a development vendor, pay attention to both technical and soft skills and make sure that there’s a clear line of communication between you two.
Discovery Phase
When you hire a team, you will give them all the necessary information about your project, including your goals, concerns, requirements, features you want to implement, and so on. During the discovery phase, the experts will analyze this information, define what systems your EHR can be integrated with, create a feature list, and work on EHR system certification and compliance with international regulations.
Development
Following the discovery phase, the project transitions into the hands of developers, where they commence transforming your concept into a tangible reality. Typically organized into sprints, each dedicated to a specific aspect of the project, the development process unfolds. Furthermore, all features undergo rigorous testing conducted by Quality Assurance (QA) engineers to guarantee flawless performance and a secure system.
Integration
Next, developers integrate your EHR system with other solutions that are essential for your work. The list of solutions is agreed upon during the Discovery stage. Some of the systems that can be used include:
- Health Infomation Exchange (HIE) Networks. Facilitating the secure sharing of patient information among healthcare entities, HIE networks enhance interoperability and streamline communication.
- Radiology Information Systems (RIS) and Picture Archiving and Communication Systems (PACS). Integrating RIS and PACS ensures efficient management of radiological data, offering a comprehensive solution for imaging workflow and storage.
- Laboratory Information Systems (LIS). The integration of LIS optimizes laboratory operations by managing sample tracking, test results, and data exchange between the laboratory and the EHR system.
Patient Portals and Personals Health Record (PHR). Patient portals empower individuals to access their health information, while PHRs allow patients to actively engage in managing and tracking their personal health records. - Billing and Revenue Cycle Management Systems. The integration with billing and revenue cycle management systems streamlines financial processes, ensuring accurate billing and efficient revenue management.
- Electronic Prescription Drug Monitoring Programs (PDMPs). Integration with PDMPs enhances prescription monitoring, providing healthcare professionals with real-time access to patient medication history to support informed decision-making.
Release
After completing development, the EHR system enters the Release stage, where it becomes accessible for use. This phase involves deploying the system to its intended users, ensuring a smooth transition from development to active implementation. It marks the culmination of efforts to deliver a functional EHR system ready to enhance healthcare processes.
Support
The Support stage comes next, demonstrating an ongoing commitment to the EHR system’s reliability and functionality post-release. This phase establishes a dedicated support system to address issues, respond to queries, and adapt to evolving user needs. It reflects the developer’s dedication to ensuring the continued effectiveness of the EHR system, providing regular updates, enhancements, and proactive support measures for a resilient and user-friendly solution in the dynamic healthcare landscape.
The Technology and Team Required for EHR Development
The success of your EHR system relies on two main factors; the features you choose to integrate and the technology and team behind these features. Let’s take a look at the tech stack you need for developing a custom EHR and the structure of the development team.
Here’s what a perfect team should look like:
- 2 front-end developers, one back-end developer
- 1 Android EHR developer
- 1 iOS EHR developer
- 2 QA experts
- 1 project manager
Things to Consider When Building an EHR Software
As the landscape of healthcare undergoes a digital transformation, the development of Electronic Health Record (EHR) software becomes a crucial focal point. Building an EHR system demands careful consideration of various factors to ensure its effectiveness, security, and seamless integration into the healthcare ecosystem.
Getting the EHR Compliance and Certifications Ready
Ensuring your Electronic Health Record (EHR) system aligns with stringent regulations such as the Health Insurance Portability and Accountability Act (HIPAA), General Data Protection Regulation (GDPR), Health Level Seven International (HL7), and other pertinent standards is a fundamental step. Non-compliance with these regulations not only poses the risk of severe penalties but also leaves your EHR system vulnerable to potential security breaches, compromising sensitive patient information. Therefore, meticulously navigating and adhering to these regulatory frameworks is paramount, not just for meeting legal requirements, but also for safeguarding patient data and maintaining the trust and integrity of the healthcare system.
Data Migration
The process of transitioning from your existing Electronic Health Record (EHR) system to a cloud-based, storage-supported one necessitates a meticulous approach to data migration. Effectively migrating all essential data ensures the seamless transfer of critical information to the new platform. Adopting a milestone strategy becomes paramount in this endeavor, where data is methodically transferred incrementally. This strategic approach minimizes disruptions and acts as a safeguard against potential data breaches.
Track the EHR System Performance
Monitoring the performance of your Electronic Health Record (EHR) system is a critical aspect of ensuring its continued efficiency and reliability. This stage involves implementing robust mechanisms to track various performance metrics, including system uptime, response times, data accessibility, and user experience. By continuously evaluating and analyzing these metrics, healthcare providers can identify potential bottlenecks, optimize system functionalities, and swiftly address any emerging issues.
EHR Development with IntelliSoft
In the ever-evolving landscape of healthcare, the significance of digital solutions in delivering efficient and high-quality care cannot be overstated. At IntelliSoft, we specialize in tailoring software solutions to precisely align with the distinctive needs of healthcare organizations.
Our team of seasoned developers comprehends the intricacies of the healthcare industry and harnesses cutting-edge technology to create solutions that elevate patient care, streamline operational processes, and uphold compliance with regulatory standards. With a dedicated focus on EHR development, we embark on a journey to redefine healthcare technology, empowering organizations to embrace a future where precision, efficiency, and patient-centricity converge seamlessly.
Contact us, and let’s transform your healthcare institution into an innovative and automated center of excellence.