Today, every industry and sector is rapidly evolving. The same goes for healthcare technology, where the seamless exchange and processing of data can revolutionize patient care and enhance operational efficiency. At IntelliSoft, we bring over 15 years of extensive industry experience. We are well aware of the challenges that healthcare organizations encounter due to the isolated nature of their systems. Our solution? Fast Healthcare Interoperability Resources, or FHIR, published by HL7. These specifications are crafted to foster improved data interoperability across various systems.
The significance of the FHIR data standard is highlighted by its inclusion in the 21st Century Cures Act, which mandates its use to achieve a cohesive approach to data management. What does this mean for you? Adopting an HL7 FHIR standard allows you to streamline the intricate process of aligning clinical information with standardized data formats. This enhancement will boost the flow and availability of vital health information.
In this article, we want to discuss the basics of FHIR resources to help you understand their formats, benefits, and the critical importance of mastering them for any healthcare organization striving to streamline operations and improve patient outcomes.
Table of Contents
What is the FHIR Meaning?
In the complex healthcare industry, where information is as vital as the treatments given, a streamlined method for managing and exchanging this data is essential. Today, Fast Healthcare Interoperability Resources play this role. FHIR resources are the foundational building blocks of healthcare data, enabling systems to communicate more fluently and efficiently.
The FHIR meaning can’t be overstated. It divides healthcare data into manageable, standardized categories such as patients, laboratory results, and insurance claims. Each of these categories is encapsulated in the HL7 FHIR standard. These resources are carefully crafted to specify the data elements they include and outline the constraints on these data and their interrelations. This organized method ensures that healthcare systems can effectively exchange and understand each data piece.
Consider the Patient Resource as an FHIR standard example. This resource contains crucial details such as the patient’s basic demographics, contact information, and links to relevant clinicians or organizations. What sets the HL7 FHIR standard apart is its use of common World Wide Web technologies. Each resource is linked to a unique Uniform Resource Locator (URL), making it readily identifiable and accessible within any system that complies with HL7 and FHIR standards.
The modular nature of the HL7 FHIR standard is truly remarkable. These resources can be utilized individually or collectively to address a wide range of healthcare scenarios. This versatility is crucial in the dynamic and varied field of healthcare.
FHIR Resource Data Formats
On the technical side, FHIR standard healthcare resources are noteworthy for the data they hold and how they are formatted and integrated into existing systems. These resources are typically available in several data formats, such as XML, JSON, and RDF/Turtle. Each follows strict logical structures and definitions derived from the Reference Information Model (RIM). The data maintains its integrity and intent across various platforms and technologies regardless of the format.
Each resource is uniquely identifiable by a URL, which helps pinpoint its exact location within the system and enhances interoperability. Alongside each resource is a set of metadata crucial for FHIR search operations and cataloging data, thus aiding the efficient retrieval and management of information. Additionally, resources include an XHTML summary that offers a brief, readable overview of the contents, accessible even to those without deep technical expertise.
The definitions within each resource ensure that every data element is clearly understood, maintaining clarity and consistency across different implementations. The extensibility framework within Fast Healthcare Interoperability Resources, designed specifically for healthcare applications, allows for the resources to be extended and customized to meet specific needs, ensuring that FHIR can keep pace with the evolving demands of healthcare.
Benefits of FHIR Resources in Healthcare Integration
The influence of Fast Healthcare Interoperability Resources on the healthcare sector is profound. FHIR is making seamless data sharing across various healthcare systems a reality. Let’s discuss the concrete benefits of these resources and how they are reshaping healthcare integration.
Standardized Data Exchange
A key advantage of FHIR resources is their ability to standardize data exchange. As a universal language for healthcare systems, Fast Healthcare Interoperability Resources enable accurate and effortless information communication. With a consistent data format, diverse systems developed with different specifications can easily understand and share information. No need for complex and costly conversions, which is crucial in healthcare, where precise data interpretation can mean the difference between life and death.
Increased Interoperability
FHIR resources are modular and extensible. These features significantly improve interoperability among healthcare platforms. This design approach helps bridge the gaps between varying data formats and reduces the longstanding issue of data silos in healthcare IT.
The modular structure of FHIR allows for incremental implementation, enabling healthcare providers to adopt new functionalities without needing to overhaul existing systems. This gradual integration supports smoother transitions and enhances communication between older and newer technologies.
Flexibility
Flexibility is another significant advantage of Fast Healthcare Interoperability Resources. Whether employed individually or as part of an FHIR bundle, this standard offers a resource for nearly every clinical or administrative need. This versatility allows healthcare organizations to customize the technology to suit their specific requirements, such as managing patient records, scheduling appointments, or processing insurance claims. Moreover, as new demands emerge from new healthcare services or regulatory changes, Fast Healthcare Interoperability Resources can quickly adapt by developing new resources or modifying existing ones.
Better Security
Unfortunately, data breaches are increasingly common today, and ensuring the security of patient information is more important than ever. FHIR resources incorporate strong security mechanisms to safeguard patient data during exchanges. Additionally, this standard supports the integration of SMART on FHIR apps, a framework that utilizes the OAuth 2.0 standard for secure authorization. This system protects data and eases the implementation of security measures, freeing developers to concentrate more on functionality and less on crafting custom security solutions.
Through these advantages, FHIR resources support a more interconnected, secure, and efficient healthcare environment. The importance of this standard in promoting effective communication and data exchange across the ecosystem is set to grow, stimulating innovations that improve patient care and operational efficiency.
Key Components of FHIR Resources
Fast Healthcare Interoperability Resources have transformed how healthcare data is structured, exchanged, and utilized. To fully leverage FHIR in any healthcare system, it’s vital to understand the structure of a resource. Each resource is intricately designed with key components that ensure its functionality, extensibility, and effectiveness across diverse healthcare scenarios.
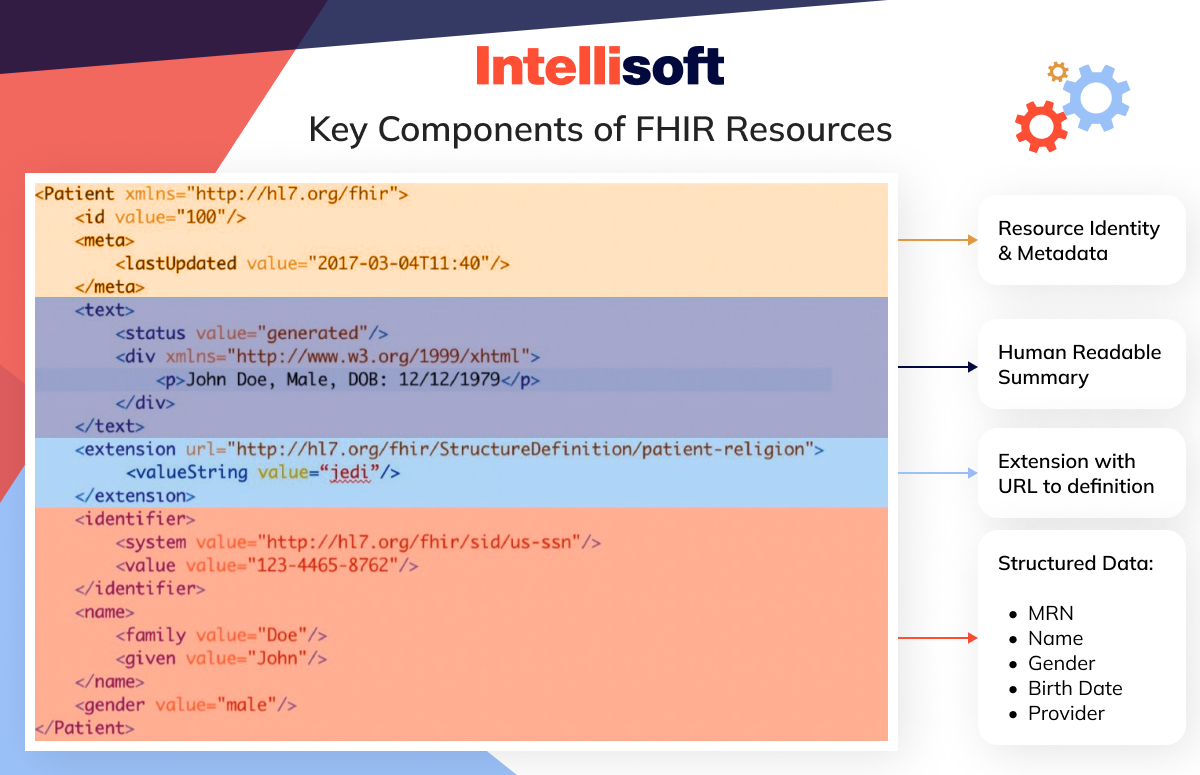
Resource Type
At the core of each FHIR resource is its type. This determines the kind of resource, Patient, Observation, Medication, etc. The resource type is crucial as it defines the structure and the expected data, guiding its interactions within the ecosystem. Each resource type is tailored with specific data elements to fulfill its intended role effectively.
ID
An essential feature of each resource is its unique identifier that facilitates referencing and updating within the system. This ID is necessary to track resources across various processes and maintain data consistency during system interactions.
Metadata
Alongside the ID is the resource’s metadata, which includes vital details such as the resource’s version, its last update, and security labels. Metadata is instrumental in resource management, supporting version control, and enhancing data security.
Common Elements
FHIR resources include several common elements that standardize and enhance interoperability:
Implicit rules outline the construction rules of the resource, ensuring consistency in creation and interpretation.
Language indicates the language in which the resource is presented, which is vital for applications in global healthcare settings.
Narrative provides a human-readable summary of the resource, typically in XHTML format, making the data easily understandable.
Extensions
FHIR also accommodates customization through extensions. These extra properties can be added to resources to include data that the standard FHIR specifications do not cover. Extensions ensure that resources can meet various healthcare requirements without altering its core structure.
Modifier Extensions
Modifier extensions are special extensions that can alter the meaning or interpretation of a resource. They are used judiciously to maintain the integrity and foundational definition of the resource while offering flexibility for specific scenarios.
Data Elements
Data elements are specific to each resource type and convey crucial information. For instance, the FHIR Patient resource might include details such as name, birthdate, address, and contact information. These elements are precisely defined to meet healthcare providers’ needs and ensure accurate and efficient data exchange.
Search Parameters and References
FHIR search parameters enable efficient querying and retrieval of resources based on their data elements, which is essential for managing data effectively within large systems. References link resources together, creating complex data structures that mirror real-world relationships. For example, linking an FHIR Encounter resource to a Patient resource shows who was involved in a medical encounter and provides a clear patient history.
Contained Resources
FHIR also allows resources to be nested within others, known as contained resources. This feature enables a comprehensive data package to be compiled in one location, reducing the need for multiple requests or external data retrieval.
Related readings:
- Comparing HL7 vs FHIR: Core Differences
- Step-by-Step Guide to Developing HIPAA-compliant Medical Apps
- Transforming Healthcare Communication: Integration of HL7 Interface Engine
- Telemedicine App Development: Features and Key Phases
- What Technologies Are Driving the Health Protection System?
FHIR Resources Structure
The structure of Fast Healthcare Interoperability Resources, as established by HL7, demonstrates the framework’s commitment to consistency, modularity, and interoperability. This design simplifies the representation and exchange of health data, ensuring that resources can communicate effectively within and across different healthcare systems.
Consistent and Modular Design
The essence of FHIR’s design is its consistent and modular structure. Each resource is designed to operate independently with its own data and functionality, yet it can integrate seamlessly with other resources to form a comprehensive system. This modularity is essential, as it allows developers and healthcare providers to add or update functionalities without extensive system modifications, facilitating easier updates and scalability.
Unique Identifiers and Interactions
A critical feature of FHIR’s structure is using unique identifiers (IDs). Every resource has a unique ID that facilitates identification within the system and supports its referencing, updating, and retrieval. This is crucial in healthcare settings, where precise patient information tracking and updating are vital for delivering effective care. These IDs ensure that each data piece within the standard ecosystem is easily accessible and manageable, boosting the system’s overall efficiency and reliability.
Supporting a Range of Clinical Use Cases
FHIR is built to accommodate a wide array of clinical use cases, with its standards including over 157 well-defined resources. These resources span various healthcare aspects, such as patient information, providers, care plans, diagnostics, medications, and financial details. This extensive coverage ensures that nearly any clinical scenario can be documented and managed within the standard framework.
Grouping and Clinical Narratives
While individual FHIR resources can effectively function independently, they can also be grouped into clinical documents. This functionality allows for a holistic view of a patient’s data, providing healthcare professionals with comprehensive insights into a patient’s health status and history. Besides, resources can reference each other to create detailed clinical narratives, which are crucial for building a complete patient profile, enhancing understanding, and improving continuity of care.
Resource-Specific Structures
Although all FHIR resources adhere to a general framework, the specifics may vary significantly based on the resource type. As an FHIR example, a Patient resource contains different information and functions differently than a Medication resource. The specification offers detailed documentation for each resource type, explaining its structure, intended use cases, and interactions with other system parts. Each resource is utilized to its full potential and maintains proper interaction with other resources, upholding the efficiency and integrity of the healthcare data ecosystem.
FHIR’s structured approach makes it an effective tool for managing healthcare information and ensures adaptability to healthcare’s constantly evolving needs.
Common Types of FHIR Resources
With 157 distinct FHIR resources available, healthcare professionals involved in data management and patient care must understand the most commonly used types. These resources are categorized based on their function and utility within the healthcare data ecosystem. Let’s discuss these common types and highlight their importance in enhancing healthcare service quality and efficiency.
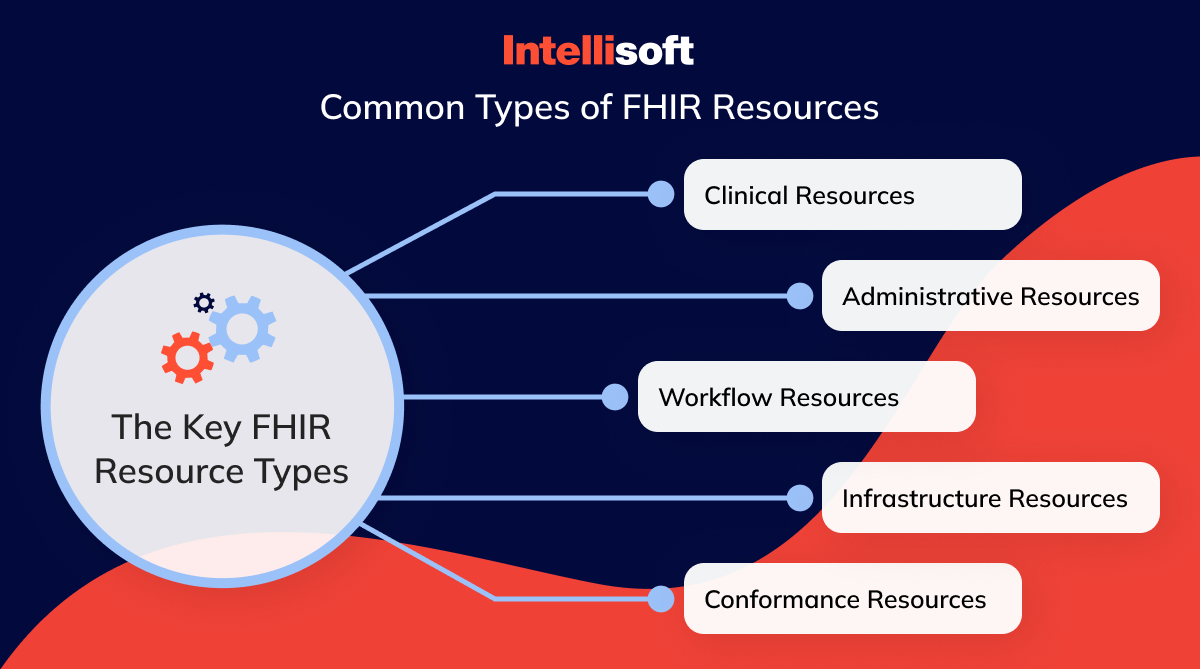
Clinical Resources
Clinical resources are fundamental to patient-related data in healthcare systems, documenting medical events, conditions, and treatments a patient undergoes during their care journey. Key clinical resources include:
- Observation. This type of examination captures measurements and findings related to a patient’s health status, such as vital signs, lab results, and clinical assessments.
- Medication. Details the medicinal products prescribed or administered to a patient.
- MedicationRequest (formerly MedicationOrder). This is crucial for proper medication management, as it represents an order for a medication to be dispensed or administered by a patient.
- Condition (or FHIR Condition, formerly Problem). Documents medical conditions, diagnoses, or significant health events needing attention.
- Procedure. Records procedures performed on or for a patient, from surgeries to counseling sessions.
- DiagnosticReport. Summarizes the findings and interpretations of diagnostic tests, providing a comprehensive view of patient diagnostics.
- Immunization. Tracking a patient’s vaccination history and status is key for preventive healthcare.
- CarePlan. Outlines strategies and protocols to address the specific healthcare needs of a patient.
These resources ensure comprehensive recording, easy access, and seamless integration of patient health data across health IT systems.
Administrative Resources
Administrative resources are vital for the foundational information necessary for all healthcare processes. These include:
- Patient. Captures essential details about a patient, such as their name, date of birth, and other demographics.
- Practitioner. Provides information about healthcare professionals involved in care delivery.
- Organization. Details about healthcare institutions such as hospitals and clinics.
- Location. Specifies where care is delivered within a healthcare facility.
These resources are crucial for smooth and efficient healthcare systems, facilitating quick access to fundamental patient and provider information.
Workflow Resources
Workflow resources are crucial to organizing and managing healthcare processes, from patient appointments to task assignments. Significant workflow resources include:
- Task. FHIR Task manages specific actions needed within the healthcare setting, such as administering medication.
- Appointment. Coordinates the scheduling of patient consultations and visits.
- ReferralRequest. Manages the referral process to another healthcare professional.
- Order. Issues instructions for healthcare services like lab tests or imaging.
These resources are fundamental in ensuring that each step in the healthcare delivery process is well-coordinated, thus minimizing delays and reducing potential errors.
Infrastructure Resources
Infrastructure resources support and enhance the functionality of the healthcare data system. They include:
- StructureDefinition. Dictates how different resources are structured.
- CapabilityStatement: Outlines the capabilities and functions supported by a system, promoting compatibility.
- SearchParameter. Enables effective searching and filtering of data within the system.
- MessageDefinition. Defines rules for specific types of data exchange messages.
These resources ensure that all parts of the health IT ecosystem can communicate and function effectively.
Conformance Resources
Conformance resources help maintain standardization and interoperability of health information technologies, ensuring that all systems adhere to the same guidelines and can interact seamlessly. Important conformance resources include:
- CapabilityStatement and StructureDefinition. Define system capabilities and resource structures.
- ValueSet. Specifies permissible data values for different elements, ensuring consistency.
- OperationDefinition. Details the operations and functions that can be performed within the system.
By setting clear standards and protocols, conformance resources ensure reliable and efficient data exchange between different healthcare IT systems, supporting the integrity of patient care across the board.
These resources collectively enhance healthcare systems’ ability to effectively manage patient information and care processes.
Types of FHIR Implementation
The versatility of Fast Healthcare Interoperability Resources allows for various implementation strategies depending on an organization’s infrastructure and strategic goals. Whether an organization chooses a basic implementation to meet immediate regulatory requirements or a more comprehensive integration to enhance data management and analytics capabilities, understanding the two primary types of FHIR implementation can guide the best path forward.
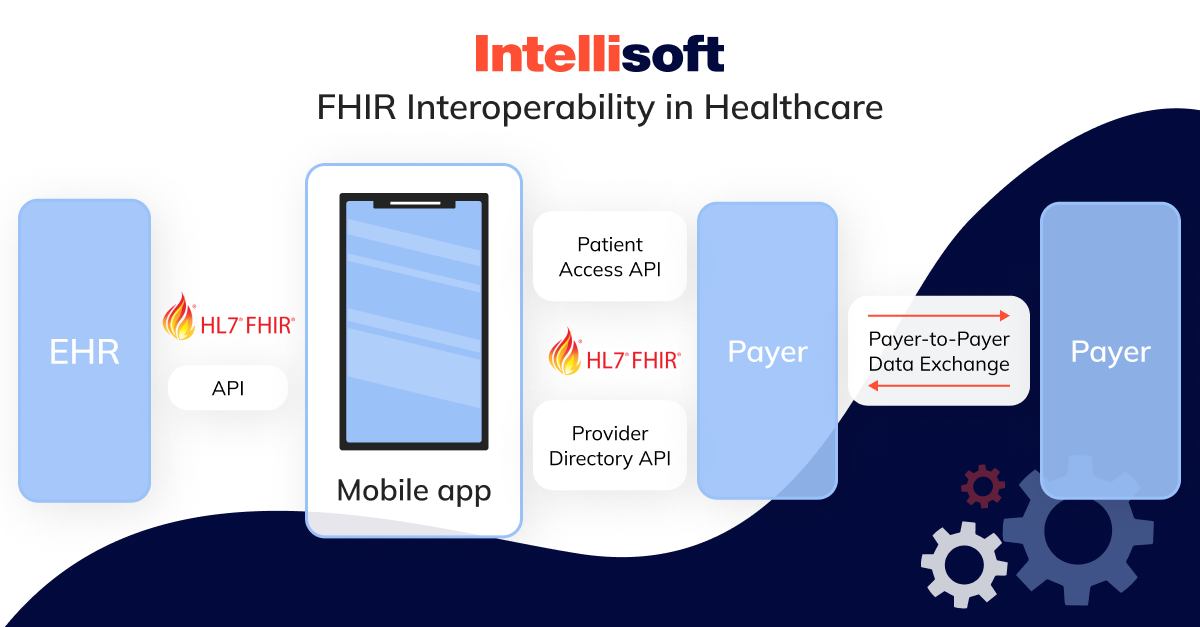
FHIR API Standard on Top of an Existing System
Many established healthcare systems with ingrained technologies opt for implementing an FHIR API standard over their existing systems. This method balances compliance with interoperability mandates without requiring a complete IT infrastructure overhaul.
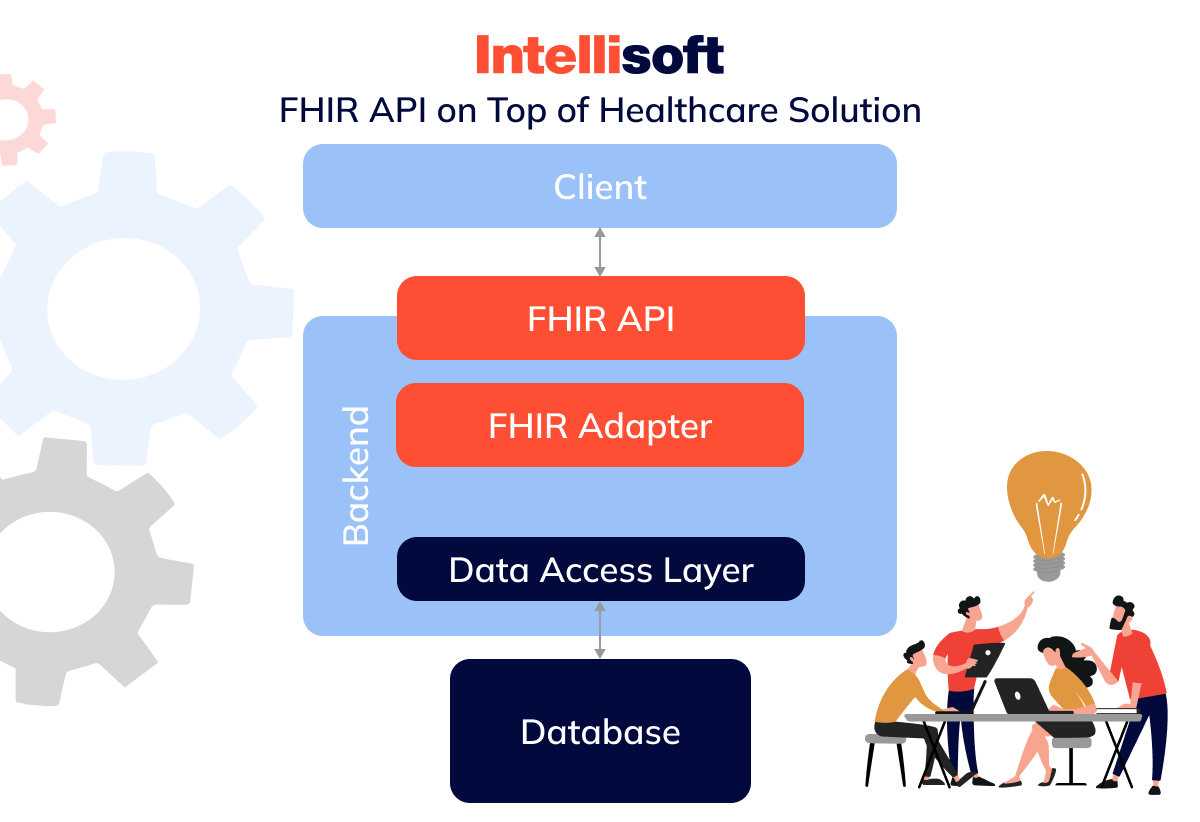
This implementation typically involves four key layers:
- Proprietary database houses all the existing data.
- The data access layer is an intermediary facilitating access to data stored in the proprietary database.
- An FHIR adapter or facade is crucial for converting data from the system’s native format into resources. It often utilizes middleware from third-party providers known for its efficiency and compatibility with various healthcare data models.
- FHIR API is the external interface through which resources are accessible. It enables integration with the broader FHIR ecosystem, including applications that support SMART on FHIR for enhanced functionalities like decision support and advanced analytics.
This model enables healthcare providers to maintain their existing data systems while benefiting from standard’s enhanced interoperability and compliance features.
Native FHIR System
Adopting a native FHIR system might be beneficial for organizations looking to build new systems or significantly revamp their healthcare data management.
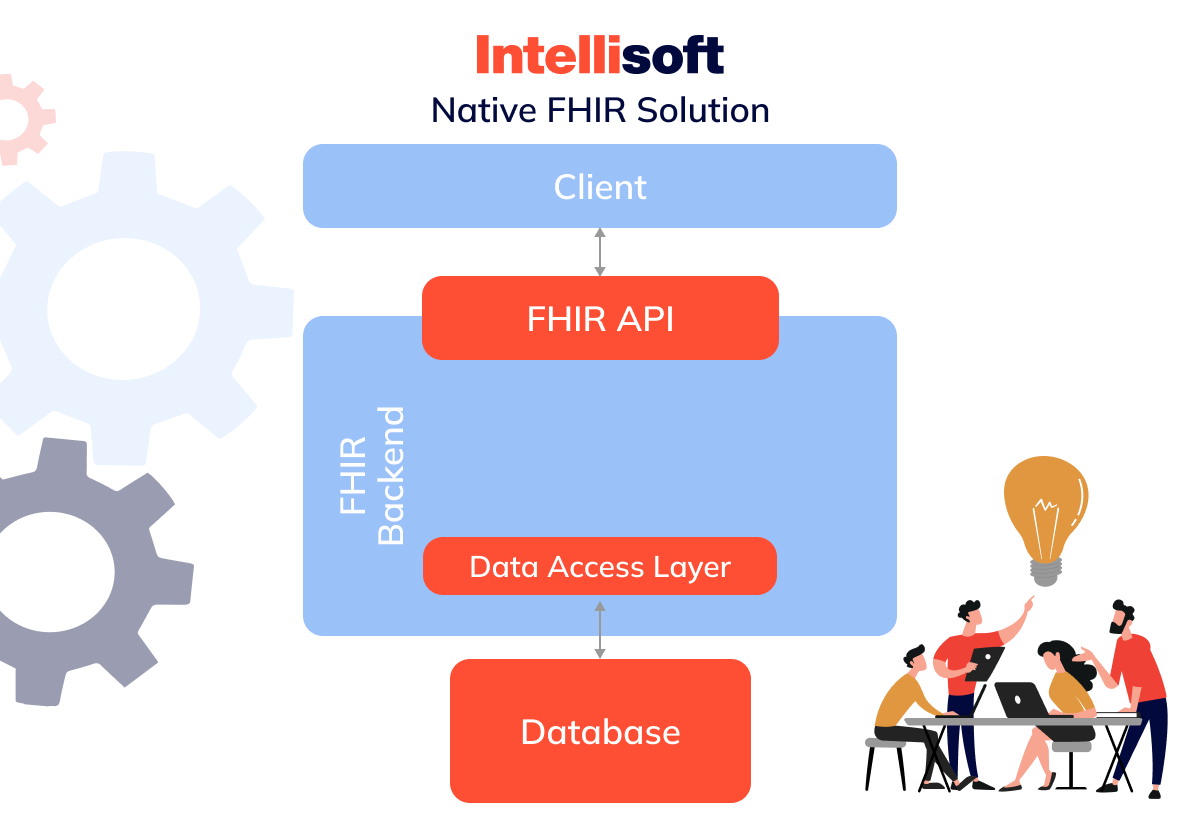
In this approach, the system is designed around standards from the beginning, utilizing resources, profiles, and extensions as core data model components. This strategy is especially advantageous for:
Prototypes and New Products
Startups and new healthcare ventures benefit from FHIR by bypassing the complex processes of defining custom data models speeding up product development and market entry.
Alternative Data Storage
FHIR also serves as an efficient data storage solution, useful during transitional phases of system development, or when temporary storage solutions are required, allowing data to be directly stored in standard formats without investing in custom data adapters.
While a native FHIR system offers a future-proof solution that minimizes translation errors and maximizes system compatibility and efficiency, it demands careful planning and expertise. It’s most effective when implemented with technology providers skilled in FHIR systems. They can ensure the system meets current requirements and is well-prepared for future advancements in healthcare technology.
SMART on FHIR
What is SMART on FHIR? It’s a standard that marks a significant evolution in healthcare interoperability. Originally designed as a standalone standard to address interoperability challenges, similar to FHIR, SMART (Substitutable Medical Applications, Reusable Technologies) has shifted its focus to enhance implementations. This strategic pivot has greatly influenced the development and integration of FHIR-based applications within healthcare systems.
As the standard became more prominent within the healthcare community, SMART adapted its mission to support this emerging standard. It has become a comprehensive framework and ecosystem supporting building, deploying, and managing FHIR-based applications. This adaptation has enabled SMART on FHIR to provide essential infrastructure, including documentation, software libraries, and sandbox environments, all facilitating the development of interoperable healthcare applications.
SMART on FHIR offers significant benefits to both healthcare providers and software developers:
For Healthcare Providers and Patients
The primary aim of SMART is to create a dynamic marketplace for healthcare applications similar to those seen in the travel or financial services industries. This marketplace enables healthcare providers and patients to seamlessly switch between various apps that integrate directly with their Electronic Health Records (EHRs).
For Developers
SMART on FHIR provides developers with a solid technical framework, including open specifications and profiles that dictate how specific data types, such as medications, allergies, prescriptions, and conditions, should be handled. These specifications, often based on standardized coding systems like SNOMED, simplify the development process by reducing the complexity and workload for developers crafting healthcare applications.
The integration of SMART on FHIR into the healthcare ecosystem has created numerous applications that significantly enhance patient care and data management. Examples include mainstream applications such as FHIR Epic, Apple’s Health app, and Microsoft Azure FHIR API, which utilize the SMART on the FHIR platform to provide advanced healthcare functionalities to consumers and healthcare professionals.
Preparing for FHIR Adoption: Challenges and Solutions
Adopting the Fast Healthcare Interoperability Resources standard marks a significant advancement for healthcare providers aiming to boost interoperability and compliance. Yet, transitioning to FHIR-ready systems introduces challenges that necessitate thoughtful planning and strategic solutions. Here, we delve into some key hurdles and their solutions to facilitate a smooth implementation.
Patient Matching
Patient matching, or identity matching, is crucial for linking a patient’s data across various healthcare systems to create a comprehensive health record. This task is essential for interoperability but comes with considerable risks. Inadequately performed patient matching can result in serious issues, including HIPAA violations and potentially life-threatening medical errors. A notable problem is the absence of official tools for efficiently identifying duplicates and errors, often leading to manual data handling and increasing the likelihood of mistakes.
Implementing a Master Patient Index (MPI) offers a solid resolution to the patient-matching dilemma. An MPI, or EMPI (Enterprise Master Patient Index) for broader applications, is a database that consolidates patient data from multiple sources. It utilizes advanced algorithms to detect relationships between data elements, enhancing patient matching accuracy. Healthcare providers are encouraged to explore MPI options provided by EHR vendors or consider developing a custom MPI tailored to their specific needs for better control and precision in patient matching.
Security
FHIR does not inherently include mechanisms for ensuring data security, which is critical for maintaining HIPAA compliance. Consequently, healthcare organizations are tasked with implementing their own security measures, such as authentication, access control, input validation, and robust data management policies. This requirement can be overwhelming, particularly for organizations lacking a specialized IT security team.
Adopting SMART on FHIR can significantly mitigate these security challenges. SMART FHIR incorporates support for authorization and authentication protocols, effectively bridging the security gaps in the framework. For healthcare providers unsure of their capability to manage security independently, utilizing SMART FHIR presents a straightforward and dependable method to secure their implementations.
Lack of Infrastructure
Although FHIR facilitates broader integration with the app economy, it does not provide the technical infrastructure necessary to support such integration. This shortfall can hinder the standard’s adoption, posing challenges for healthcare providers and vendors who require robust system architectures to manage and utilize the standard effectively.
Fully managed FHIR cloud platforms offer an advanced solution to the infrastructure challenge. Leading tech companies such as Amazon, Google, Microsoft, IBM, Salesforce, and Apigee have developed enterprise-grade cloud platforms for implementations. These platforms provide a full array of services, including API management, data storage in FHIR format, PHI security, and analytics connectivity.
Cloud platforms handle the operations, maintenance, and compliance aspects, simplifying the deployment of FHIR services in the cloud. Organizations new to cloud technology or those seeking expert assistance will find partnering with a technology provider to implement these cloud solutions extremely beneficial.
By tackling these challenges with well-considered solutions, healthcare organizations can effectively manage their transition to FHIR, boosting their interoperability capabilities while ensuring compliance and security. This preparation facilitates smoother operations and sets the stage for more innovative and efficient healthcare services.
Conclusion
Adopting Fast Healthcare Interoperability Resources is becoming increasingly critical as the healthcare industry moves toward more integrated and interoperable systems. FHIR promises to streamline healthcare processes and improve the accuracy and accessibility of patient data across different platforms, ultimately enhancing patient outcomes. However, transitioning to this standard involves several challenges, including issues with patient matching, security concerns, and the need for a robust technical infrastructure.
At IntelliSoft, we fully understand the complexities involved in implementing FHIR. We are well-equipped to guide and support your healthcare organization’s journey to adopt this standard or provide your personnel with FHIR training, helping them achieve FHIR certification. Our team of experts is skilled in delivering tailored solutions that meet your specific needs. By partnering with us, you can tap into our extensive expertise in cloud technologies, ensuring that your healthcare systems meet the latest standards and are at the cutting edge of technological innovation.
Contact us to revolutionize your healthcare data management and take a significant step forward in your organization’s digital transformation.